Why is it necessary
for the chronically ill patient to keep a detailed symptom
diary?
by Marie Kroun. MD - 2010
In
order to judge if the patient suffers from a currently active
Borrelia infection and/or other co-infections, the doctor will need the
patient to write down a very detailed
disease history,
including details on the risk of or known exposure to tickbite or to
other bloodsuckers, travel history (previous possible or known exposure
to "exotic" infections? - some malaria forms may recrudesce years after
the primary infection), if the patient has given blood or
has received blood (since the subject
is blood infections some of them may be transmited by blood
transfusion for certain, for instance Babesia),
plus the patient must deliver necessary data for evaluation of any
previous test result (photocopies of original test results,
doctors papers)
- this is both in order to check if
other explanations / diseases for symptoms has already been
evaluated for and ruled out or treated for, and for evaluating if
previous test results have pointed to exposure to Borrelia
and/or
other infections - this tells about what has been in the
past
- but the doctor will
also need an overview over the current symptomatology and
severity
/ degree of disability, to judge the need for treatment, and which
treatment might help the patient best.
The current
symptomatology can be visualized on symptom scores and
log curves via the Excel symptomdiary (english
& danish
version), which is a free download and may be used by any chronically
ill patient to keep track of his/her symptoms / treatment result,
provided the copyright is not violated by changing the diary, except as
advised in the "how to use" description.
After a while (1-4
months) the symptom curves may display a recurrent relapse
pattern suggesting the patient could be suffering from a currently
active Borrelia infection, so the
cyclicity can be taken into consideration for when is the best
time to sample blood for direct detection of Borrelia spirochetes!
-
to understand why that is, some scientific background
information
of spirochetes and their alternative forms may be needed, see
http://lymerick.net/MK-videomicroscopy.html
The main observation was that
the characteristic
Borrelia relapse patterns probably reflects the
age of the cysts, since Brorson's found that young Borrelia
cysts produced new "baby" spirochetes in about 9 days (clinically
6-14 days), while old
cysts took about 4 weeks (clinically 3-6 weeks) to reconvert to
spirochetes.
Illustrative
relapse pattern curves, but only over total score are shown below, but
in the
diary are also curves per individual symptom, and sum per organ system
- so it is
possible quickly to see if and how individual symptoms develops /
swings over time during ongoing flare
and which symptoms
eventually swings together
or develop in series over days ...
Burrascano was the first to note the monthly relapse pattern characteristic of Borrelia burgdorferi
infection during antibiotic treament, and found that there was a high
risk of quick big relapse, if the patient stopped the antibiotic
treament as long as there still was a noticeable flare cycle, so
he recommends to treat Borrelia infection initially for at least 4
weeks - in order to break a whole lifecycle - and to continue treatment
until the flare cyclicity ceases
- see his latest guidelines at ILADS website: http://ilads.org/lyme_disease/treatment_guidelines.html
Burrascano's
important observation was supported by findings in my long
term follow-up study on patients enrolled which displayed a current
activity / relapse cycle on their symptom diary, and who came out
positive on direct fluorescent specific immune stain for Borrelia burgdorferi.
The symptomdiary /
relapse pattern can be used to spot when is the
optimal time for sampling of blood for microscopy (and for culture and PCR), since
spirochetes are
especially found in the blood within the first 24 hours after
the start of a new symptom flare-up.
The chance of finding spirochetes by microscopy (or catching some of
them in the sample for culture, PCR) in a randomly taken blood sample,
i.e. when the investigator can NOT take the individual
patients relapse cycle into consideration, is at best around
10% (1/10) in a "weekly" relapse cycle, but only 3% (1/30) in a monthly
relapse cycle, i.e. much tedious blood microscopy time / expensive
materials (BSK-H, Bb-specific antibodies for direct immune stain,
primer for
PCR) can easily be wasted in "not finding", if the patient don't keep
the Excel symptomdiary for at least one month (weekly cycle)
to
four months (monthly cycle); at least three relapses are
needed in order to judge if there is regular and recurrent flare
activity, so the blood investigation can be planned to when the next
time a flare is supposed to set in.
The symptomdiary is very useful for getting the patient and the doctor
good overview over a complex symptomatology and long term ongoing
disease proces, no
matter what the cause(s) is/are, since it can be used to evaluate and
follow
any chronic disease long term, and be used for documenting effect /
side effects of any tried intervention, whether it is traditional
medicine or alternative. A patient doing long term diary daily
also shows very good compliance. Only very compliant patients
will
be suitable for participating in research studies on testing and treatment for infections.
The visual analog
symptom scale used in MKs symptomdiary resembles NYHAs 4 degrees classification of the
disability in heart disease (minus 1), the scale is:
0: normal; patient do not need to write zero scores
in diary,
nothing is added to the total score if patients feels perfectly normal.
1: mild disease i.e. slight limitation of activity
2: moderate disease i.e. marked limitation of activity
3: severe disease i.e. debilitating/incapacitating symptoms even during
rest.
However, it is very important that patients score each
individual symptom in floating
point values - at least gives half and quarter
point-scores - otherwise the 4 point scale is not sensitive enough to
show minor flare activity changes.
Now
to some real-life Borrelia flare activity patterns:
More
information on the 33 first 'pilot' project participants overview here: http://lymerick.net/York2003/projpatients.pdf and Powerpoint-presentations:
York2003-PPT, York2004-PPT (#11 and #24), Leicester2007-PPT i.e. case #49
and #50):
NOTE There are
always 7 days between the shown dates on the X-axis, i.e. one
week. The left Y-axis is the symptom score and the right
Y-axis may
show antibiotic dose levels (later version of the diary program).
NOTE also that counting the daily/nightly
number of urinations and
defecations gives around 10 point/die normally as part of the
total score; so
be aware if the patient keeps track of these or not! - since it is not
possible to reach a ZERO total score, if the patient IS keeping track
of the number of urinations and defecations; daily
and nightly urinations should be counted because some patients
have signs of reduced antidiuretic hormone (ADH or vasopressin)
secretion, especially noticeable during night time where ADH
should peek in order to reduce urine excretion in order not to
disturb the patients night sleep; lack of ADH excretion during
night may lead to excessive nightly (and daily) urinations, which
again lead to
increased thirst; so be aware of an important objective
sign: if the patient
always
carries a water bottle and drinks from it and refill it
often, and immediately needs to spot where the toilet is,
because of need for frequent urinations, there could be such a problem!
...
in that case it is important to measure the amount of urine
production over time and note when urinations occur / and the amount of
urine produced during both day and night, at least for some days,
including during flare-up time,
because patients
report such symptoms especially during neuroflare time! ~ if very high
urine excretion can not be reduced (urine concentration can be
measured, osmolality) by reducing the water
intake (Addis fluid deprivation test), it may be true diabetes insipidus
and
investigation of other hypophysis hormones may be needed also. If there
is lack of ADH and frequent nightly urinations desturbing the patients
night sleep, leading to fatigue, the patient may be helped by nasal vasopressin spray
(Minurin) at bedtime, just like the bed-wetting smaller children, where
the nightly ADH peak is not ocurring. While children usually don't wake
up on urination reflex and wet their beds during sleep, adults often
will wake up on the urge urination reflex and go to the toilet;
severe debilitating fatigue during daytime may be improved / prevented
just by taking away the patients urge to pee and thus wake up 2-3 times
every night!
The number
of defecations and the "quality" of the stool must be noted
because most pt. will develop some degree of diarrhea
as adverse effect during antibiotic treatment, and because patient may
have "irritable bowel" symptoms as part of their disease picture.
Borrelia burgdorferi
and alike spirochetes has been detected in biopsies from the bowel
system: http://lymerick.net/Gastrointestinal-spirochetosis.htm
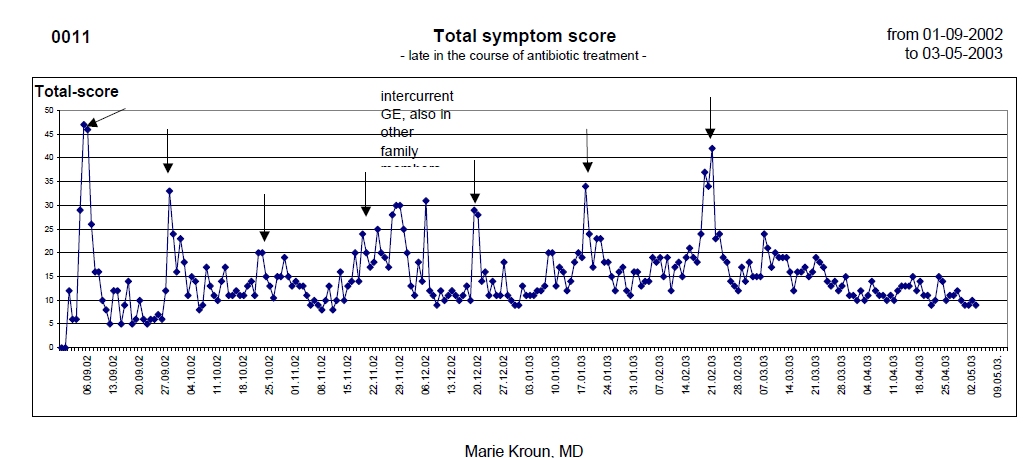
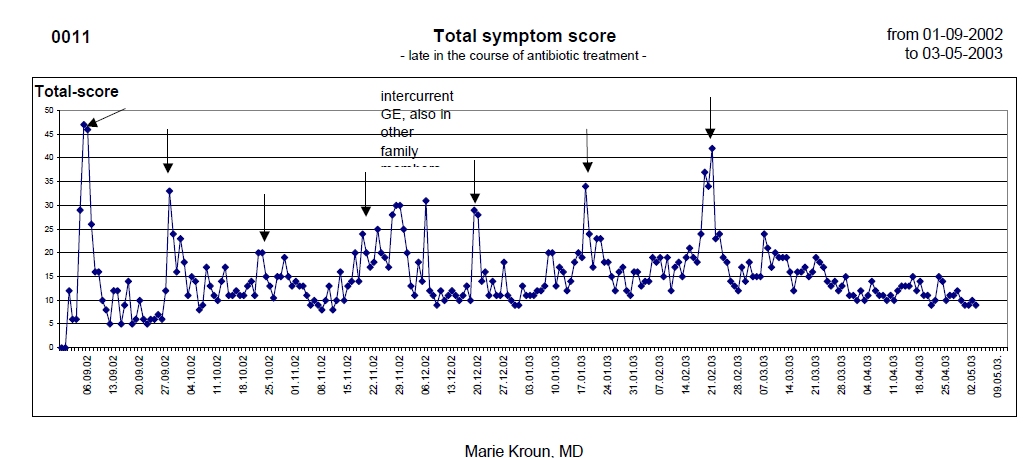
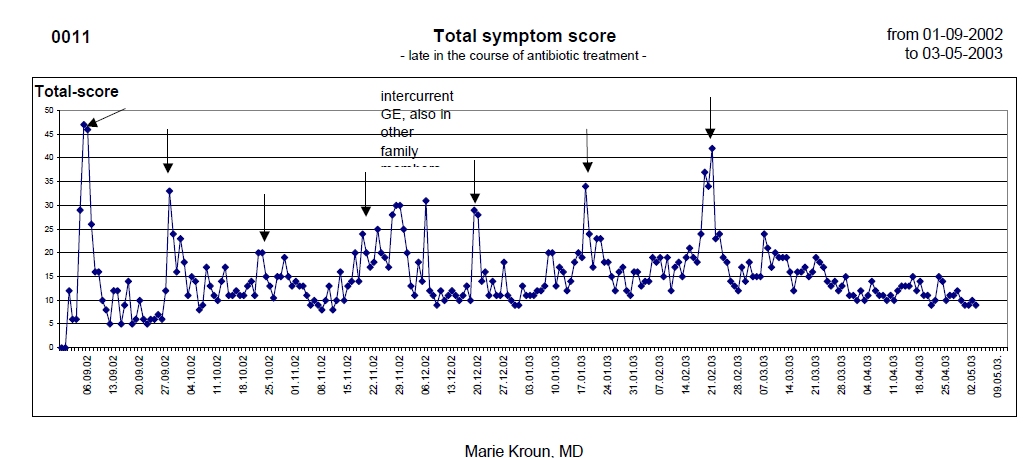
#11
(above) showed a monthly
relapse cycle, with high scores during flares, but
low/normal in between flares ..
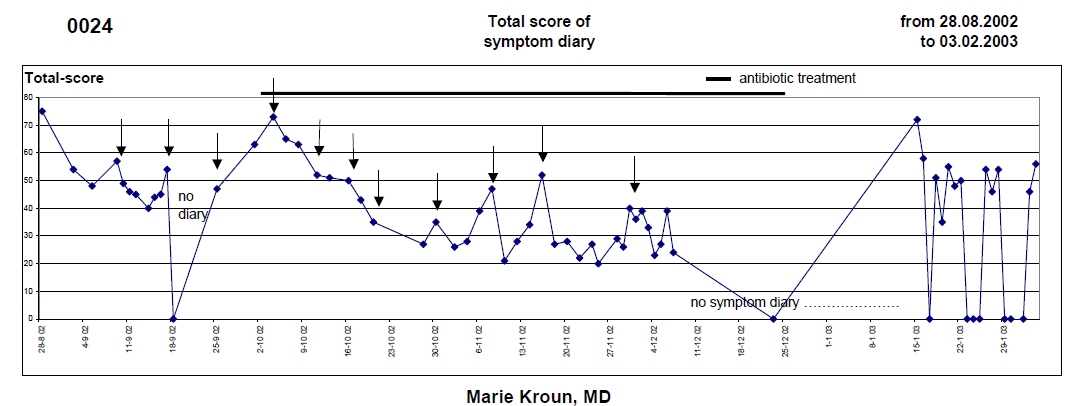
#24
(below) shows
one month diary with weekly
cycle before direct fluorescent antibody test for Borrelia
burgdorferi, which came out positive, plus pt. also had ringformed
babesia-like
parasites in red blood cells; then shows the start of
antibiotic treatment (metronidazole and
azithromycin); note the Herxheimer-like worsening for a few days
into the first treatment week and thereafter gradual
improvement, as usually seen during the first 3 months of
antibiotic treatment especially in patients with Borrelia, but
without sign of co-infections; co-infections may fluctuate in a
different pattern, overlying cycles blur the curves and if the
co-infection is not found / not targeted by antibiotic treatment, the
course may be slow / improvement much less than expected - so look
out for / test for co-infection, if the patient does not respond
as expected on antibiotic treatment known to target Borrelia, but not
intracellular co-infections, like penicillin, amoxycillin, ceftriaxone
(cell-wall antibiotics) ..
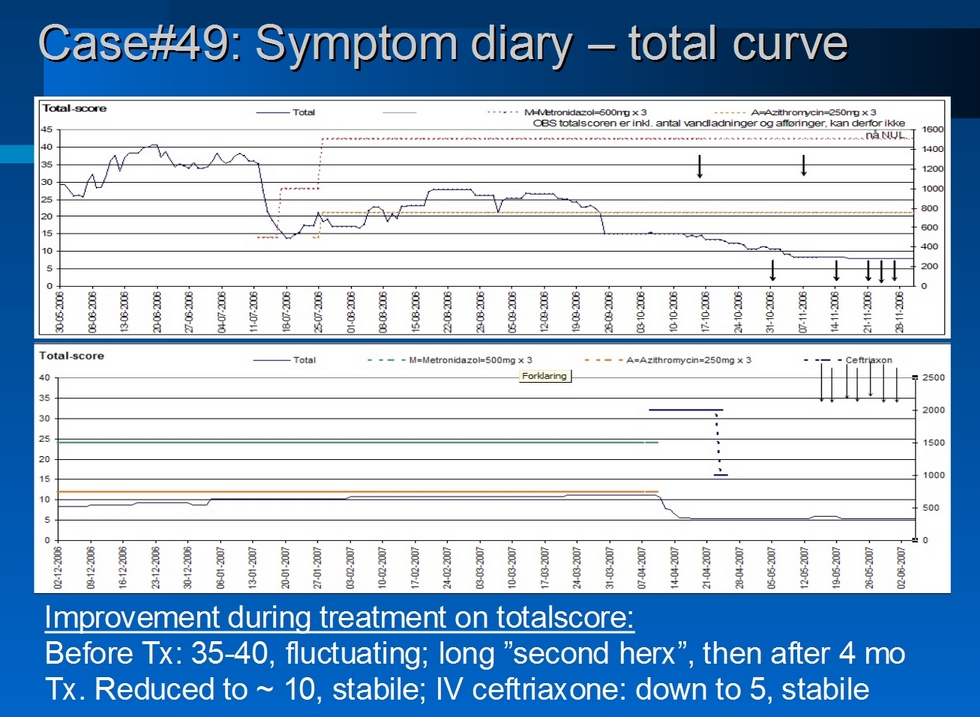
Some patients may experience a rather long "2nd
Herxheimer"-like worsening reaction,
possibly those with a very high load of hitherto dormant Borrelia cysts
on stock in tissues, that dependent on the age of the cysts
(?)
enter growth cycle in a more or less steady flow, until all the younger
cysts have been cleared and only older cysts are left to give monthly
relapse pattern.
This is illustrated in #49:
Observations from the project
showed that often a borrelia
flare starts with a rectal
temperature drop of 0.5-1 ºC down
to 36.0 ºC or even below
- usually in
the late afternoon, compared to that particular pt. normally
has
37.0-37.5 ºC at
that time of the afternoon, when measured outside flare time and
compared to the
normal temp. range measured in rectum.
Must be measured with same thermometer and this must be checked againt
other thermometers for a correct and realiable measure. Oral, ear
or skin measurements is NOT reliable enough to measure the small
temperature variations!
In the danish project participants diaries their rectal temp. usually lies between 36.5 to
37.5 ºC
outside flare time, lower in morning, higher in afternoon and evening;
during female ovulation and premenstrual phase plus 0.5 ºC, but there may be individual variations.
Concurrent with the temp. drop
the patient often feel chilly and malaise, often have to
go to
bed with clothes on to get warm, extremities may
feel cold and have a bluish color - cyanosis,
eventually as livedo reticularis -
i.e. signs of uneven / reduced circulation in the skin, and the patient
may
also begin to have certain "start of neuroflare" markers
- usually
the patient has some characteristic sensory disturbances or pains,
brainfog, blurred
vision / reduced contrast sensitivty (this can be
objectively measured
by FACT or VCS online); within 6-12 hours
after start the
patient feel like getting a fever and temp. may have been
raised by 1-2 ºC,
but due to the previous temp. drop, the pt. temp. usually only reach
the subfebrile
area (37.5-38.0 ºC).
Around
2-3 days after start of flare symptoms are usually dominated
by
"reactive symptoms" possibly due to reduced vascular blood flow /
vasculitic
problems, signs are:
The histopathological
Hallmark of Borrelia infection is perivascular infiltration with
chronic inflammatory cells, probably
elicited by precipitation
of circulating
(IgG) immunecomplexes,
the amount of which was shown to fluctuate with the
symptomatic
relapses of Borrelia in joints; damage of
endothelial cells may also
be mediated by TNF/TNF-alfa signals induction of programmed cell
death, apoptosis?
In
order to combat intracellular infections the host immune system
need to kill all his/her own infected cells, preferably at a
time when the infectious agents are not mature, while the
infectious agents on the other hand may try to hold the host cell
breakdown until they are mature and ready to infect neighbour host
cells; some of the intracellular microbes - that are associated
with chronic persistent intracellular infection - may interfere with
the host cell response to TNF apoptosis signal by activating NFkB delaying the host cell breakdown?
Also
Borrelia can exist both extracellularly and intracellularly and
may survive intracellularly at least for a while during treatment with
cell-wall antibiotics like penicillin and ceftriaxone - http://lymerick.net/Bb-intracellular.htm
- that is probably why treatment only with IV ceftriaxone and
penicillin may fail, and why some doctors recommend to follow-up
after IV treatment with antibiotic treatment that can penetrate better
into deeper tissues and intracellularly than the "penicillins", i.e.
with drugs like the tetracyclines (tetracyclin, doxycyclin,
minocyclin), the (3th and 4th generation) makrolides (clarithromycin,
azithromycin) and metronidazol (which may both penetrate well to
tissues (cross blood-brain barrier) and may be able to break the
spirochete-cyst-spirochete life cycle (Brorson on metronidazole PMID: 10379684) ...
TNF
can be measured increased during Jarisch-Herxheimer reaction, and
during Borrelia activity; Shoemaker found that high TNF-alfa correlated
with reduced retinal bloodflow (measured by Heidelberg doppler
flowmeter) and with reduced Functional Acuity Contrast Test (FACT) in row C-D-E, see http://chronicneurotoxins.com and http://biotoxin.info ... read more about FACT at http://contrastsensitivity.net
Shoemaker measures a lot of cytokines and hormones like MSH in his research, and was the first to show that C3a and C4a (complement split products) can be
raised in borrelia infection as early as within 96 hours after an
infecting tickbite!
Result
of attack on vascular lining, leading to inflammation and blood
clotting (eventually thrombus formation leading to infarct) is
reduced blood flow, which again can
explain some of the most common symptoms of borrelia infection:
- muscular
pain / quickly developed
"acid feeling in muscles" on excercise
(short walking distance); low blood flow =>
quick exhaustion of the cellular energy depots and
insufficient oxygen
transport to the cells, may lead to anaerobic cellular
metabolism, i.e. puruvate ending
in lactate
instead of becoming
a substrate for Krebs cycle, and
reduced transport of carbondioxide away from the area; combined can
such factors readily explain why the patient quickly burn out and why
the muscles feel like having run a marathon race; the hallmark
of chronic fatigue syndrome (ME/CFS) is quick exhaustion, very slow
regeneration; the recovery proces after exercise
that take a normal
person few hours may take days in the CFS pt. because of very
slow
replenishment of the energy depots after they have been used
up; read
the biochemistry lectures on
energy metabolism: pyruvate ATP cellular respiration Krebs cycle ...
- likewise
the mental functional
problems /
neurocognitive problems, that most borrelia (and
CFS) patients have,
may also be due to reduced brain blowflow; indeed SPECT may
show
reduced blodflow in areas responsive for handling
the functions that are reduced; the functional reduction can be
measured objectively by thorough neuropsychological testing and assessment
(microbesandmentalillness.com); read
Vance Spence 2005 lecture in Sheffield
conclusion from several studies: "ME/CFS
is pro-oxidant and proinflammatory" (as a
resume in danish by
MK
with SPECT and other pictures brought w/permission from VS)
...
Many
proinflammatory
markers
can be measured and found increased in chronic
inflammatory conditions; but unfortunately lack of access
to laboratory methods / lack
of money can prevent the thorough evaluation that chronically
and
complex ill
patients really need for getting a proper MEDICAL evalutation, at least
before diagnosing psychiatric disease of unknown origin!
I get insight in papers and test results from many patients and thus have documentation enough for stating that many
chronically ill patients have not been evaluated properly for
inflammatory disease/infections, before their symptoms are
being
labelled "psychic" or "stress induced"; mostly patients
only get "routine measures" and chronic inflammatory disease
is outruled, when CRP and SR is not found elevated; these measures
are often not elevated in chronic Borreliosis and other slow infections!
It
puzzles me how doctors dare treat chronic inflammation like rheumatoid
arthritis, inflammatory bowel disease etc. with anti-TNF drugs, without
proper evaluation for infections and without ever measuring the by the
treatment targeted TNF niveau before and during the anti-TNF treatment,
which may have very severe adverse effects!?
How thorough chronically ill patients with variable multi-organ-system symptoms should be evaluated can be detucted from the Biotoxin pathways chart: http://www.biotoxin.info/images/BiotoxinPathway.pdf
- which also gives hints to treatment modalities for some of the common symptoms ...
read short about Shoemaker's innovative work and his websites http://chronicneurotoxins.com
http://biotoxin.info
...
Lyme
borreliosis patients (and patients with other infections of the nervous system, most wellknown in syphilis) may
have severe neuropsychological problems on top of physical disabilites
or
mental illness may even be the sole or major
manifestation of their
Lyme borreliosis; the neuropsychological problems are probably
an
effect of proinflammatory cytokines
/ interleukines
which are raised as the hosts immune response to infection;
cytokines can induce behavioural changes, for instance when
cytokines
are
injected into animals (PDF);
the animals express about the same "sickness behaviour" as
does humans ... withdrawal from the flock (light and noise
sensitivity makes it unbearble for the patient to be among a noisy
crowd), anhedonia,
aggression, anxiety,
fatigue/lethargy, anorexia, sleep disorders ...
Inflammation/cytokines
can also result in hormonal changes for
instance lead
to reduced MSH
- along with reduced ACTH hormone, lack of ACTH lead to less
stimulation of the adrenal gland cells, i.e. reduced
cortisol production, less ability to
tolerate stress? ... reduced melatonin => sleep
disorder, important for the seasonal / diurnal rythm ...
Robert
Bransfield, psychiatrist and current president of
ILADS (2010), have recently given very interesting presentation with
lots of
references on the subject of psychoimmunology, but this was too much
to give you a review of here ..
Indeed,
neuro- psycho- endocrino- and immunology are always combined, are not
separate functional entities,
thus the division
of
doctors into different types of medical specialist does not fit the
natural
build / human functions very well, but has tended to create quite
narrow-minded
doctors,
that focus within a very small area of their special interest
in medicine.
Chronically ill
people with multi-organ-system disease / symptoms need generalists that
read science from many specialities, knows enough to understand
the pathogenesis / can explain the disease symptoms, and who can test
appropiately and who can treat all found infections and hormonal
dysfunctions etc. - or at least the patient will need to consult a team build
of INTERESTED people, who co-work on
evaluation of these complex patients;
since many (chronic) (intracellular)
infections starts the very same immune responses leading to the same
"unspecific" symptomatology, it is important to not only focus on
"borrelia or not?", but think of all possible causes and evaluate the
patient thoroughly, because treatment options differ depending on which
infection(s) is/are involved in starting and maintaining the immune
cascade reaction ...
It
may be that some patients do not downregulate
a raised proinflammation situation normally, and some patients
have been found to express certain genetic markers, i.e. some of their own
tissues / cells express antigens that are
alike some microbial antigens - molecular / antigen mimicry
- thus antibodies resulting after
infection with certain microbe(s) may raise an
inflammatory response, that can begin attacking
self; read for instance PMID: 15695691 PDF...
-
and if
the hosts own molecules / antigens alone - after the infectious
agent(s) has been eradicated - can continue to stimulate continued
formation of
antibodies that continue to react with self antigens, the patient has
developed an autoimmune
disease!
Which genes are responsible, and why don't these patients
downregulate
inflammation normally and are more vulnerable to certain infections, that are
the question wee need to find answers for! ...
thus persistent symptoms after antibiotic treament is not always due to
persistently active infection, but persistent infection will of course also
continue to
induce continuous antibody formation, that may bind to the patients
microbe antigen alike tissue antigens, and keep the inflammatory proces rolling.
(Chronic) Borrelia
patients may express elevated ANA, RF and other autoimmune markers,
though usually not on a level high enough for diagnosing autoimmune
diseases like lupus or rheumatoid arthrtis; moreover these measures can
fluctuate with disease activity and normalize after improvement on
antibiotic treatment. Such patients may have prolonged "reactive
symptoms" much longer than do people who do not express alike genetic
markers?
We will never able to find out what makes some,
but not all the (Borrelia) infected sick, unless we have access to lab
tests and can evaluate each patient thoroughly - like dr.
Shoemaker does - with all the most modern "state of the art" test
methods!
Doctors "art" is to be able to
disciminate between causes and it is necessary to be able to
discriminate, because treatment options / what will work best for the
individual patient are very different, depending on the pathological
mechanisms involved.
The most important question for the patient and the clinical doctor
- who treat the patient - are then very important for the
decision of which treatment:
- are symptoms induced by persistent infection
that need treatment with antibiotics and where
the use of immune depressive drugs can be very dangerous to
the patient, or
- is it solely an autoimmune process that
need to be treated with immune
suppression, or
- is it a combination of autoimmunity
/ antigen
mimicry i.e. both cross reactions and continuing infection both
at the same time, so
the patient may benefit from taking immune depressing drugs
under
cover of antibiotic treatment, to prevent persistent infection from
fluorishing during the immune despressive treatment?
- the symptoms are alike,
but
the treatment is very different and making the wrong treatment choice
may not only not help the patient, but may harm and even kill the
patient, in case of severe immune depression is created by medical
intervention, that fuels the underlying infection, which can fluorish
whenever corticosteroid or other immune depressive treatment is
not done under concurrent antibiotic treatment. There are published
case reports and I've also personally seen patients, who - after
primary Borreliosis apparently recovered well after antibiotic
treatment or spontaneously, i.e. who for years were asymptomatic
or only had had occasional "minor" flares, who was treated with
high dose prednisolone or similar drugs due to suspected autoimmune
disease due to found elevated measured of autoantibodies, who crashed
totally after the corticosteroid treatment and from which Borrelia
antigen then could be detected in their blood during the relapse by
direct detection methods!
Therefore
I recommend that "previous" Borreliosis patients should never be
treated with corticoid steroids or other immune depressants, unless the
patient also is treated prophylactically with antibiotic
treatment, to prevent microbes from multiplying during time of severe
immune depression!
Symptoms are elicited by the
immune reactions
raised every time a group of spirochetes enters blood circulation and get
attacked by the immune system
- i.e. the chronic Borrelia patient usually experience recurrent relapses coming at
intervals. There can be longer latent periods with fewer symptoms, but patients are often not asymptomatic.
Every kill off of several spirochetes during treatment will
elicit fierce immune reactions - including / induced by elevated
TNF; the worsening reaction seen during treatment was named
the
Jarisch-Herxheimer
reaction after the doctors describing the worsening reaction
during syphilis treatment.
It is very important to tell the
patient that a worsening reaction can be expected and is sign that
spirochetes are being killed, i.e. that the treatment works, it is NOT
A SIDE EFFFECT. Also when a patient does not "Herx" at
all, the
treatment
may not help in the longer run either, thus is indication for a
re-evaluation, perhaps a change of treatment; the first Herx
reaction can be very bad in high
bacterial load, hence high bacterial kill, but can be reduced and be
more tolerable by starting antibiotic treatment with low dose and wait
increasing
the dose until the reaction has worn off in usually a few to 5 days.
Many patient explain a very abrupt "turn-off" of the Herx reaction, as
switching the light of. It is also necessary for chronically ill
patients to understand that worsening reactions will occur every time
a group of new spirochetes emerge from stock of hitherto dormant cyst
forms
entering growth, i.e. recurrent worsenings can be expected during
treatment, just like in the
untreated active disease pattern, until the stock of Borrelia cysts has
emptiet itself.
Burrascano was the first to tell
about
this in his guidelines already back in beginning of the 1990ies. For
unknown reason the second Herx is often the worst/longest (see #49 above), and usually
starts around
the 3-5 treatment week, and may last from a couple of weeks to
6
weeks or even longer, fluctuating on a high symptom level (often up to
75% of
what the level was before treatment); the pt. who felt a very
good
improvement
in week 2 and 3, and before the second Herx sets in, can get
very
disappointed and feel very depressed
during the second worsening phase, think the treatment does
not
work after all, that bugs have already developed resistancy to
the
drug, or that (s)he has very bad side effects from the
antibiotic
treatment
- however, the stock of hitherto dormant cysts can only be
reduced and finally
emptied, whenever some of them enter growth phase, form new spirochetes,
that wanders to the blood
circulation and create complement cascade and cytokine storm
and thus symptoms; unfortunately only active bacteria in growth can be hit by
antibiotics, when the metabolic processes are active that antibiotics
interfere with; some
patients gets so depressed that they are in suicide risk during
the Herx phases, especially if not having been
prepared for
the 2nd Herx in advance! -
patients need much psychological
support from their peers and a doctor, who
knows all about this from experience, can say
"others felt likewise bad for a while, so just hang in
there, it will get better, but it may take up to 2-3 months to get
through it".
After
the 2nd Herx phase, most Borrelia infected patients usually stabilize on a lower
lag-phase (50-100% symptom reduction compared with level before start
of treatment)
and then shifts to a monthly relapse cycle, relapses coming only from
old
cysts, in time - as the stock of growth-able cysts reduces - relapse
tendency eventually fade away, less intensive and eventually
longer intervals.
The first week Herx can often be
avoided by starting low dose and gradually increase the antibiotic, but
the second Herx - the younger cysts emptying phase (?) -
unfortunately has to be tolerated;
stopping or lowering the dose may increase risk of bacteria
developing resistancy to the drug(s).
Herx'es are far worse on bactericidal
antibiotics (killer drugs), less on bacteriostatic
treatment (growth inhibitors), i.e. the Herx is sign that some bacteria
is being killed giving waste product that trigger cytokine storm, i.e.
that the drug(s) works, so it is actually a good sign! - a relatively long second Herx phase is illustrated above in curve
from #49 in the 2007 Leicester, UK PowerPoint (cases #49 and #50).
Patients
experiencing a very bad and very long 2nd Herxheimer reaction have
usually been sick for years (> 2 years) before Borrelia
diagnosis and
treatment, and they may take long time to have lasting
improvement and no
more flares.
Monthly flare activity
can continue for years, each giving
a risk of big relapse (to the level as before antibiotic treatment or
worse) if stopping
the antibiotic treatment, at a time when the
patients immune system alone can not suppress the new spirochetal
growth sufficiently; tell the patient to count on it
may take just as long to
empty the stock of
dormant cysts, as it has taken to fill the stock with them!
BUT
#11 (first curve above) who was already on social security sick pension
for a couple of years and used a wheelchair for severe
"chronic fatigue syndrom" and could neither do much physically, nor mentally,
before the diagnosis and
treatment of Borrelia, plus sign of two co-infections (ringforms
in
red blood cells, and morulae-like / ehrlichia-like inclusions in white blood cells) -
after above curve - still had flares, but at 3-6 monthly intervals
until 2005, where she stopped the antibiotic treatment, which she only took
during flare activity; she has had no flares needing antibiotics
since. She could begin working for money part-time in 2005, has since taken a
new
education, as a dietist and is feeling great now - has a life that is worth
living again!
The cure (we hope!) was
not done solely by antibiotics, but also by the patients own focusing
on her diet and other
lifestyle factors.
We are what we eat! - it
should not come to surprise to anybody that immune function
may be hampered by lack
of
essential nutrients/wrong diet, by toxin overload (heavy metals like
mercury for instance) and not the least by stress.
After years
of
chronic illness and reduced stamina, the body and mind need to be
gradually retrained in order to regain better functionality, and
learning to cope with having to live with lasting symptoms from
permanent tissue damage also takes its psychological
toll on the patient.
The danish society
(social service) is - unfortunately IMO - putting very
high pressure on
very sick people to go to work despite illness; "the system" is not
aware that it may actually hamper
the
healing process, stressing the patient so much and leaving no time nor
energy for
the patient to rebuild capabilities and learn to compensate for
lost functional
abilities. Time is needed after long term illness, but the society shut
off the economic support often already after 12 months on sick-leave
and demand the ill patient works, no matter how ill!
Recently
a danish cancer patient on sickleave, who had a good job to get back to
after treatment, was sent on "activation", as if the cancer
disease was caused by a lack of motivation to work for a living?!
#49
(above) was very lucky that his brain infarct did not give him
much brain functional defects; he clearly improved on the
peroral treatment,
yet his symptom level still reduced even more when he was put on IV
ceftriaxone! - which he was at first denied by the ID hospital doctors,
who did not believe in the test results from USA, nor do they
want to believe
in the existence of "chronic borreliosis" and usually says "there is no
evidence
that longer than 10-21 days treatment works better"
- but seing the curve from #49, I wonder if he would perhaps
have improved faster and better, if the ID doc had NOT refused
to treat
him with IV ceftriaxone at first?
... it was another
hospital department (dermatology) that around 6 months later gave
him IV
ceftriaxone treatment; he
continues antibiotic treatment via GP (because pausing treatment
make his symptoms increase); he
has improved a lot, is usually normally functioning and working full
time, but he still feels occasional very bad flares, thus dare not
risk stopping the treatment, use it as relapse prophylaxis
...
It is a huge stress factor to be chronically sick / relapsing, and then
on top be
"treated" by ignorant doctors, as if we are a bunch of crazy malingering
hypochondriacs!
- at least we can see that our symptoms
are influenced by the intermittent presence in our blood of
some
serpentine microscopic moving/swimming structures that should not be
there
-
when we know, because we can see and film the bugs presence in the
blood during activity, that our suffering come from
spirochetes cyclical acticity, not
from "imagined demons" as they think
- we realize that antibiotic treatment is the most rational treatment
... but why do we have to fight so much for it?
All doctors have to obey the WMA International code of ethics
: "shall ... respect human life", "shall act in the patient's
best interest when providing medical care.", "owe his/her patients
complete loyalty and all the scientific resources available to him/her.
", "shall be dedicated to providing competent medical service in
full professional and moral independence, with compassion and respect
for human dignity.", "respect the rights and preferences of
patients" ... etc. - yet many doctors deny the chronically ill patient
the right to try a treatment option that might help improve the
condition - why? .. it seems like Lord Nelson, who deliberately raised the telescope to his blind eye and stated "I really do not see the signal" ...
More project patients have had a
very good outcome, that seem to last for years after stopping
antibiotic treatment, but there is still room for further improvement!
- so the research work MUST BE CONTINUED :)
MONEY is needed for continued research, please donate money to http://daninfekt.dk
- the KONTINGENT subpage tells the bank account information.
Ignorant doctors will be able to continue saying "there is no proof
/evidence that longer term / different treatment works better"
-
as long as patients trying longer term / different treatment
regimens, does not register the effect of what they try, in the only
manner that can be accepted by hesitant doctors
- prospective symptom score
using a visual analog scale, combined with repeated blood evaluations
for the eventual presence of spirochetes and other abnormal findings!
It
need to be do in a way, so results can be published in a scientific
journal, otherwise it does not count, will not be read by doctors,
will not be taken into account!
ONLY
PATIENTS WHO GET DIAGNOSED WITH CURRENTLY ACTIVE BORRELIA / SPIROCHETE
INFECTION BY DIRECT DETECTION METHODS AND WHO ARE OFFERED
"EXPERIMENTAL" TREATMENT, that differs from the normally recommended
treatment, CAN SHOW THE WORLD HOW / IF THEIR SPECIALLY DESIGNED
TREATMENT WORKS BETTER, BY SYSTEMATICALLY KEEPING TRACK OF THEIR
SYMPTOMS (via a symptom diary of some
sort, MK's Excel diary is a free download, so feel free to use it!), AND BY COMPARING SYMPTOMS
WITH BLOOD MICROSCOPY ...
Frankly, I
do not understand why is it so hard for certain doctors (especially
neurologists, ID specialists and microbiologists) to accept
that chronic / persisting borreliosis is a
reality some
patients have to live with! - when these doctors know / accept
that herpes, CMV, HIV, tuberculosis, lepra and more infections
can be chronic / lifelong persistent in nature and that sick people with such
infections need treatment for many months to years, HIV even for the
rest of the infected patients lifetime, in order to suppress
the
viral growth?! ... some immune depressed Borrelia patients is
apparently in the same situation as HIV patients, but usually can't get
the antibiotic treament they need in order to suppress the microbial
growth and be able to have a better life.
Why do certain doctors ignore (no ref. / no discussion) in their
articles on Borrelia .. the many - since 1989 - reported culture,microscopy and PCR verified cases of
persistent / chronic Borrelia infections?
As
long as they continue to IGNORE THE REALITY THAT MANY SICK PATIENTS
HAVE TO LIVE WITH, patients will need to help interested researchers collect much
more data as illustrated
here
...
Several hundreds, if not thousands of patients, if possible
...
otherwise the unbeliveing doctors will continue to reject findings by
saying "well, it is
just a few exceptional case reports".
I wonder how many
successful
case
stories and how many cases of by direct detection modes diagnosed
chronic (seronegative) borrelia (relapsed) cases, it will take
to turn
"the common medical opinion"?
The Excel symptom diary has helped us spot
symptoms and exposure reactions, which the doctor might not
have
thought
of asking the patient for, and which the patient would not
spontaneously have told they have - because many symptoms are mentioned
in the chart which the patient will have to think over and
report,
if
present -- this often shines a new light on the case story /
gives a
broader perspective, and overview;
most diseases are
probably multicausal, and if not all contributing causes are
found and
addressed treatment
wise, the patient may not heal / may not get much better ..
However, there are many drawbacks with the
Excel symptom
diary, mainly people
will have to understand how a spreadsheet program works and must enter
all
data correctly
for the curve drawing to work (comma is used as
decimal point
in DK, i.e. 2.3 is
consided to
be text by
the danish Excel spreadsheet program version, no curve can be
drawn
from
text that look like numbers! - thus
patients must learn to use the danish number 2,3,
with comma
as decimal point indicator insterad - not easy for brainfoggy people
with short term memory problems ...
More tricky problems like this, unfortunately make
the Excel symptom-diary too difficult to use for very brainfoggy
people, so many give up
using the diary :(
MK
has a dream of patients instead of entering their score data into a
spreadsheet, which they must send a copy of to MK at
intervals, instead
could login to an online MySql database and enter their
data from any computer or even by a smart phone. Just like
MK can login
to
and search the LymeRICK article database and even open full text PDF
articles and
read and edit entries via SE Xperia X10 - nice ;)
The database tables, login pages and data enter system can be
easily made with PhpRunner
(which was used to create the online LymeRICK TBI article database),
but a program (MySql-Php in order to be compatible with the
PhpFusion
website) is needed to retrieve the symptomdata, do
all the
calculations and draw curves over everything, just like in the
spreadsheet program does - and if possible also make summed up statistics for all
registered patients on the fly, by pressing button.
Please contact
the webmaster, at http://daninfekt.dk
- if you can help program this in Php!