Comment by MK. These authors forget to take into consideration the
following::
- In a currently active Borrelia infection with
surplus of ANTIGEN compared to ANTIBODY, it can happen that all
antibodies get quickly trapped in immune-complexes,
so NO ANTIBODIES
ARE FREE and able to bind til the TEST FLAGELLA, which then measures
nothing, i.e false seronegative test outcome
- Hardin et al. 1979
(PDF) found amount of circulating
immune complexes in Lyme arthritis that was high in early infection,
highest in the sickest,
low/absent during
remission and fluctuated
with recurrent clinical activity
Schutzer et al. 1990 (PMID: 1967770) (which Hansen ref. in another of his publication in 1994, thus he is aware of the paper!) demonstrated Borrelia burgdorferi
specific circulating immunecomplexes in 10 seronegative active Lyme
disease cases, later confirmed by many others; references and danish
comment by MK in http://kroun.ulmarweb.dk/Borrelia-IC.html
- 1985
PMID: 3542350 mention in abstract that "Antigenic
variation between isolates may determine the differences in clinical
expression observed between cases in North America and Europe."
-
antigenic variation was already wellknown for closely related relapsing
fever Borreliae.
- 1992
Baranton et al. (PDF) publiced finding 3
genetically different Borrelia strains associated with different
clinical pictures, Borrelia
burgdorferi sensu stricto (arthritis, USA + EU), Borrelia garinii
("typical neuroborreliosis", lymphocytic meningoradiculits AKA
Bannwarth syndrome), Borrelia
afzelii (VS461; since old times associated with chronic
multi-organic manifestations, incl. joint and CNS and
even bone marrow inflammation; arthritis plus ACA has been
described in EU since 1920'ies, see some older refs. in http://lymerick.net/Bb-history.pdf
..
- 1992
Picken (PDF) published on variations in
the flagellin gene, which implicate possible resulting differences in
the flagella antigen among different Borrelia strains, so flagellin
anitbodies raised by mammal host to other Borrelia strains with differing
flagella antigens, may not be able to bind til the Borrelia afzelii
DK1 flagellin based antigen!? - hence could result in false
negative test results.
- Hansen & Lebech in J Clin Microbiol. 1992
Jul;30(7):1646-53. PDF page
1652: "B.
burgdorferi
antigen has never been detected in the CSF of patients with
neuroborreliosis." and "However, clinical experience has never
revealed the occurrence of relapses in patients with neuroborreliosis
who were appropriately treated (22, 29)." - these
postulates had
both been disproved by culture verified published cases see http://lymerick.net/persistent-borreliosis.htm
Preac
Mursic V, Weber K, Pfister HW, Wilske B, Gross B, Baumann A,
Prokop J. Survival
of Borrelia burgdorferi in antibiotically treated patients with
Lyme borreliosis. Infection 1989 Nov-Dec; 17(6): 355-9 PMID:
2613324
1.
5y boy.
July 1985 EM. Aug 1985 Lymphocytic
meningitis.
Seropositive
for IgG and
IgM, no antibodies in CSF.
Penicillin
V
orally 100000 u/kg/d, 14d. Spinal-fluid showed fewer
cells. September 1985 facial palsy,
again pleocytosis in CSF.
Doxyc. orally
2mg/kg, 10d.
Gradually CFS normalized. April 1986 relapse, Bb
was isolated from CSF after 4
weeks in
BSK-medium.
Penicillin
200000 u/kg, 22d.
August
1986 relapse/reinfection with EM and painful meningoradiculitis, Bb
antibodies now negative in
CFS and
serum. Culture
not done!
2.
49y man.
EM, typical signs of LMR-Bannwarth S developed 7 weeks later. Pleocytosis
and elevated
protein in CSF.
Both
Borrelia IgM
and IgG positive in serum.
Penicillin i.v. 20 MU/d, 10d.
Four
days after therapy normal examination
and no
complaints, CSF declining parameters, positive Borrelia-index. Three
months
later CSF normal, Borrelia-index now negative, but Bb was cultured from
CSF!
3.
26y
woman. Headache, radicular pain.
Normal
neurological exam. Multiple horseflie bites. CSF
pleocytosis and elevated protein.
Negative
Borrelia-ELISA in CSF and
serum.
Ceftriaxone i.v. 2g/d ,
10d. Improved.
7.5 month
later recurrent episodes of radicular pain, headache,
arthralgia,
fever. Normal neurological exam.
Negative
serology. Normal CSF. Bb cultured
from CFS after 6 weeks in MKP-medium.
Cefotaxime
3 x
2g/d i.v., 14d.
.... 3 skin isolates in post treatment relapses also descrihed ...
Many
more articles on culture, microscopy or PCR proven cases have been
added since, and particularly two studies
are worth mentioning in this context, because they both used DAKO EIA
(Hansen's Borrelia flagella based antibody test):
Oksi J Clin Microbiol 1995 (
PDF):
41 late (> 3 mdr.) borreliosis patients with either positive
culture
(12) and/or positive PCR (39); DAKO FL-ELISA missed 6 of 12 culture
verified cases or 24/41 (58%) of culture and/or PCR positive cases.
Strle Clin Inf Dis 2006 (
PDF): 33 in CSF culture-verified
neuroborreliosis cases; 23
Borrelia garinii (which fitted the "typical" picture of
neuroborreliosis, clinically and in laboratory measures), however 10
patients with
Borrelia
afzelii
neuroborreliosis, differed clinically only significantly in one symptom
(painful radiculitis), only 3 had been sick < 3 months; 7/10
(70%)
DAKO EIA CSF/serum index negative, despite duration of symptoms from 6
months to 7 years!
Conclusively:
Several
WARNING
SIGNS AGAINST OVER-GENERALISATION had been
published, some even before, others after these
authors - in Brain 1992 - expressed their BELIEF and claims, that
SERUM IgG measured by
their flagella antibody test
will always become positive at latest 3 months after symptom debut,
and that
all
neuroborreliosis patients will develop positive
CSF/SERUM index measured with their flagella antibody test, at latest
within 8 weeks after symptom debut
- statements since adopted by Statens Serum Institut
(SSI), the danish national microbiological reference laboratory
link
(danish), which continue to maintain these
postulates still, despite the published evidence AGAINST!
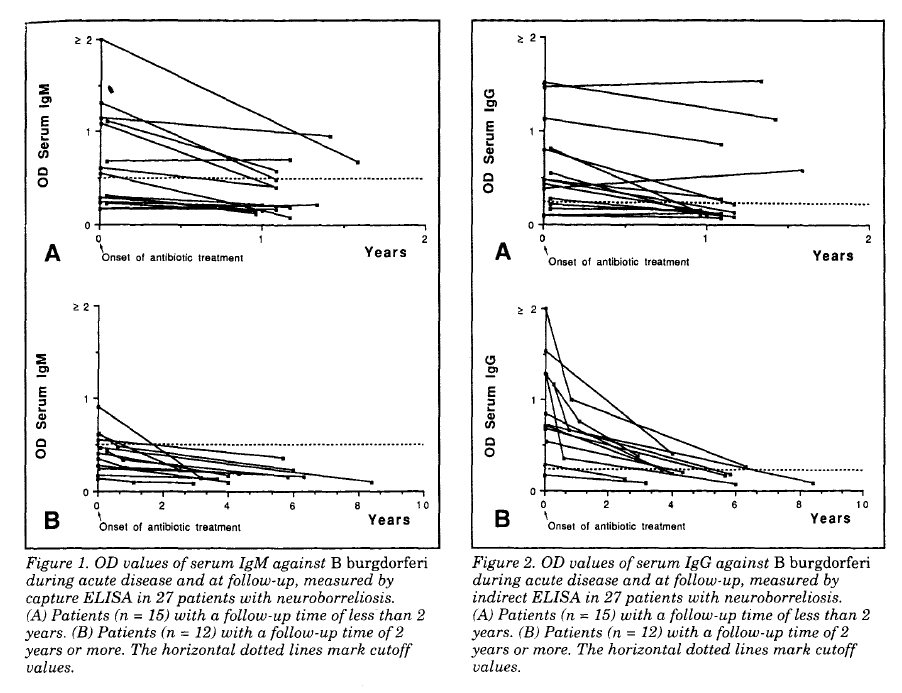
First, Hansen and Lebech have self reported a few
cases (also here!), that to their surprise, did not
develop positive Borrelia
flagella-IgG in their serum > 3 months (cases were
usually spinal
Borrelia Index positive, in this paper only IgM-index positive)!
Secondly, published works listed in
http://lymerick.net/persistent-borreliosis.htm
(available for all to see on the Internet since 2003), for
instance the paper published by Oksi et al.. in J Clin
Microbiol 1995, in which a total of 24/41 (58%) with DAKO test
measured SERONEGATIVE, BUT
CULTURE or
PCR PROVEN LATE (all sick > 3 months) BORRELIA CASES AGAINST
Hansen et al's OPINION! - plus further evidence against has piled up since
...
POSITIVE CULTURE IS THE VERY BEST POSSIBLE
MICROBIOLOGICAL EVIDENCE ONE
CAN GET FOR CURRENT BACTERIA INFECTION, and culture is often called the GOLD STANDARD
MICROBIOLOGICAL
DIAGNOSTIC METHOD!
Looking deeper into the
references which Hansen and Lebech uses to back up their statements
(sometimes they do not reference any published works), the above underlined claims
seem not to be SCIENTIFICALLY EVIDENCE BASED!
First, their main research
studies on the flagella based serology test were done
in clinically highly selected patient group, all
must express "typical neuroborreliosis" AFA lymphocytic
meningoradiculitis AKA Bannwarth S, which has (since Baranton 1992)
been found especially associated with infection with a
particular strain of
Borrelia
burgdorferi sensu lato*, i.e.
Borrelia garinii
that seems to cause more pronouced host immune and CSF reactions,
compared to other strains of Borreliae during infection of the nervous
system or without infection of the nerve system.
Next, Hansen and Lebech have (paradoxically it seems in hindsight) selected
a different strain of
Borrelia
burgdorferi sensu lato (
B. afzelii) DK1 for
their flagella antibody test, which was/is mainly intended for
diagnosing "typical" neuroborreliosis(!); it appears from their
statements that they have believed flagella antigen to be
highly conserved ~ exactly the same in all borrelia strains, at least
until Picken 1992 (which Hansen and Lebech references in 1994!) showed
the flagella gene variation among borrelia strains; but Hansen and Lebech have not
taken the logical consequence of this knowledge, which would have been
to shift test antigen to
Borrelia
garinii flagella, after the genetic differences among
different borrelia strains became revealed ...
Since, they have failed to modify
the claims, that
SERUM
IgG, measured by their flagella antibody test
method, will always become positive at latest 3 months after symptom
debut, and that
all
neuroborreliosis patients will develop positive
CSF/SERUM index , again measured with their flagella antibody CSF index
test, at latest within 8 weeks after symptom debut
- statements that were adopted by Statens Serum Institut
(SSI), the danish national microbiological reference
laboratory
link (danish),
which continue to maintain these postulates still
(checked May 2010), despite scientific evidence against and the
resulting misuse by danish doctors against have actually been presented
to SSI by me, who also pointed ouf the LACK OF DECLARATION OF HANSENS
CONFLICT OF INTEREST, over one year ago!
SSI / Hansen et al. have failed to do a similar controlled study in
culture or PCR proven DANISH LATE BORRELIOSIS CASES, as Oksi, i.e. has failed to prove with
same strengt as the opposing science, that their claims do hold; futhermore I have
suggested such a study to SSI and also suggested co-work about such
a study to the local university hospital microbiology
department, since I have access to the ideal supected chronic
Borreliosis patients for such a study in the patient society; NOT INTERESTED was
the answer from the leading microbiologist (2008)!
These authors / SSIs statements / "expert opinions" may possibly hold up for and
be somewhat justified by Hansens et al's findings done in
their specially selected group "typical" neuroborreliosis -
most probably caused by
Borrelia
garinii
- cases, that is if these authors have NOT
intentionally excluded consecutively enrolled patients clinically
suspect of having neuroborreliosis, by the fact that some
of these patients did NOT become seropositive within
their time limit ... which they very possibly might have done,
since
a positive
spinal index (within a month after symptom debut?) has often been a
strictly required inclusion criteria in several of their
studies! - thus they could perhaps have excluded some serum and/or CSF
antibody flagella antibody negative, bu truly
Borrelia infected with other strains of Borrelia, from
participating in their serology studies, which may then have resulted in
skewed results, a wrong impression!?
- thus
it seems
Hansen and Lebech have made a circular argument / conclusion (Wiki)!
The danish authors - Hansen and Lebech - were co-authors on a danish
consensus report / officially recommended Borrelia guidelines from 2006
(
link 2010 version corrected),
which fails to discuss the above mentioned caveats.
The working group
has firmly advocated using ONLY DAKO/OXOID
Borrelia flagella antibody test for the diagnosis
of Borreliosis in Denmark, the very same test which Hansen has just
(May 2010) been forced by the press (
INFORMATION.DK)
to admit that he co-owns and earns money on by sale, and which he has
"forgotten" to declare his CONFLICT OF INTEREST - that is, not only in
the Borrelia guidelines report from 2006 - but also
in other published papers, which he has co-authored,
since the rules have for a long time dictated that such a
declaration of eventual conflicts of interest is necessary for
all authors of scientific papers to send in!
Moreover, in the 2006 danish Borrelia guidelines also fails to mention
/ discuss / reference Oksi's paper, which PROVES
Hansen and Lebech's IGNORANCE of certain counter proof!
The guideline report also failed to address the important
implication of antigen trapping of some/all formed antibodies in immune
complexes, during times of ACTIVE BORRELIOSIS (early or late).
Besides the authors have twisted some statements in
the guidelines report, so it fits their viewpoint [chronic
seronegative Lyme borreliosis does not exist, stated by Hansen in
danish article in MPL 1994] a
little better, than what is actually accounted for in the
source text behind the reference; twists
that will only be noticed by readers very well into the Borrelia
literature
already and/or those who decide to check what is really stated in the
referenced source
text!
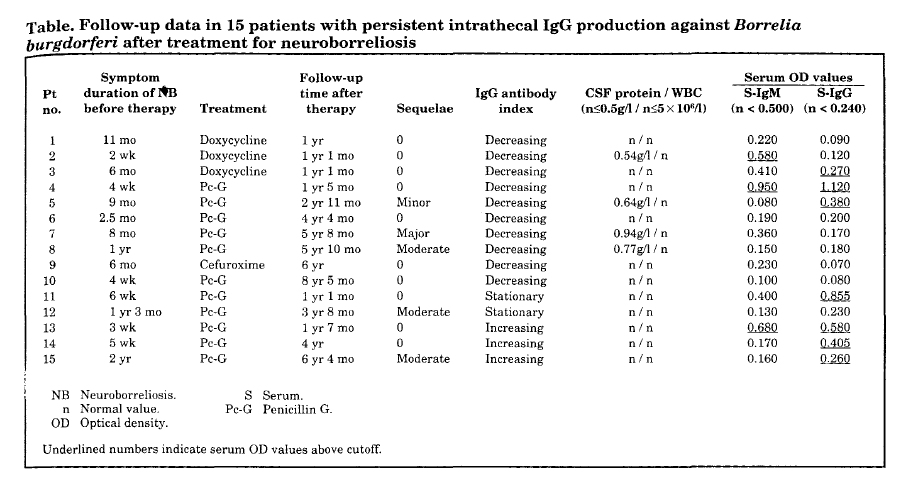
In this
paper -
Neurology. 1993;43:169-175 - Hansen and
Lebech fails to mention the very
important 1.5 time increase in IgG cut-off value,
which it seems is not being backed
up by scientifically peer-review published literature; at least I have
not been able to find the cut-off value validation that
find OD of 0.240 for IgG, in any of the sources to the sources, they
have chosen to reference as backup for the increase; most of the older
papers referenced use OD 0.160 as the 98% (some 95%) percentile cutoff value for
IgG! - therefore
the increase in IgG cut-off, does not seem to be
SCIENTIFICALLY PROVEN / IS NOT EVIDENCE BASED / IS NOT JUSTIFIED?!
WHY IS THIS INCREASE In IgG CUT-OFF NOT EXPLAINED / NOT MENTIONED / NOT
DISCUSSED AT ALL IN THIS FIRST PUBLISHED PAPER USING THE
HIGHER IgG CUT-OFF VALUE ?!
- it "smells" of a possible hidden agenda ...
We can wonder why this increase in IgG cut-off came shortly after these authors statement, that neuroborreliosis
may be ruled out - authors intention is that no further investigation of the
patient for Borrelia infection is needed - if/when the patients does
not have apositive Borrelia IgG in serum, measured by their flagella
antibody test, at latest 3 months after symptom debut
- a postulate that is very problematic, especially for the
truly Borrelia infected patients with hampered immune
function, for instance those having co-infection(s) with
immune cell infecting microorganisms, and/or have other immune
depressing co-factors involved in their disease process
- because
after
the increase in cut-off it has become 1.5 times harder for the
patient to
get a positive SERUM Borrelia IgG result?!
*) In Europe until now 6 strains within
Borrelia burdorferi sensu lato
complex has been isolated by culture or detected by PCR in European
HUMAN cases, besides
Borrelia
burgdorferi sensu stricto,
Borrelia garinii,
Borrelia afzelii,
also:
Borrelia valaisiana:
2004
EID;
10 year neuroborreliosis,
pos. PCR in CSF, seronegative. Thus is NOT ref. in the danish
guidelines report, which instead states, that human infection with
Borrelia valaisiana has not yet been proven!
Borrelia lusitaniae:
2005 PMID:
16053200,
PDF;
10 year old skin affection, culture pos., seronegative; in
the PubMed abstract is stated that the pt. never had an EM, but this wrongly was told to be EM in
the danish consensus report from 2006!
Borrelia spielmanii:
2005
EID,
culture skin EM, seronegative, lost to follow up; there are
over
100 known strains of Borrelia detected in ticks that must somehow
maintain a
tick-mammal lifecycle, which has not YET been proven to be
able to
infect and be pathogenic for humans; the perspective is that there may
be plenty of human Borrelia infection falsely outruled by negative
serology status, that we won't find out about if they are human
infective and pathogenic, until we have tests available, that are able
to detect
all the various borrelia strains; serology is highly problematic
and
will
always be problematic, because of Borreliae ability to undergo rapid
antigenic variation,
and ability to alter into more resistant alternative forms (
100 years pictorial,
Burgdorfer 1999 keynote lecture)
that may let Borrelia survice any adverse conditions, including
even long term antibiotic treatment! - later, when Borrelia growth
is no longer suppressed sufficiently, some hidden forms may revert
back to
spirochete form and cause clinical and with direct test methods
confirmed relapse of Borrelia ACTIVITY; Borrelia uses many
different tricks to evade mammal host immune attack and Borrelia
may even cause (Borrelia specific?) immune depression in LATE
infection, for instance indicated by Dorward 1997
PDF
- if Borrelia get enough time (late long tern untreated Borrelia
infection) and have success to invade and kill all the host memory
cells that are directed against Borrelia's surface antigens, this would
give a probable explanation, why so many patients, that initally
in the infection responded normally with production of
Borrelia antibodies, but which after a while, stop producing
these antibodies, despite they have clinical relapse and by direct
methods verifiable persistent and active Borrelia infection!?
WE
NEED ACCESS TO DIRECT DETECTION METHODS FOR LATE DIAGNOSED / CLINICALLY
SUSPECTED RELAPSING LYME BORRELIA CASES; such tests are not
currently supplied by any danish microbiology laboratory!
POSSIBLY PROPER EVALUATION IS BEST DONE ABROAD - in other EU countries
like Germany, which have many more Borrelia infections
yearly, therefore - compared to danish doctors - have much more
experience with chronic / relapsing Borrelia cases, than it is possible
to get for any doctors here in Denmark, where only 100-200
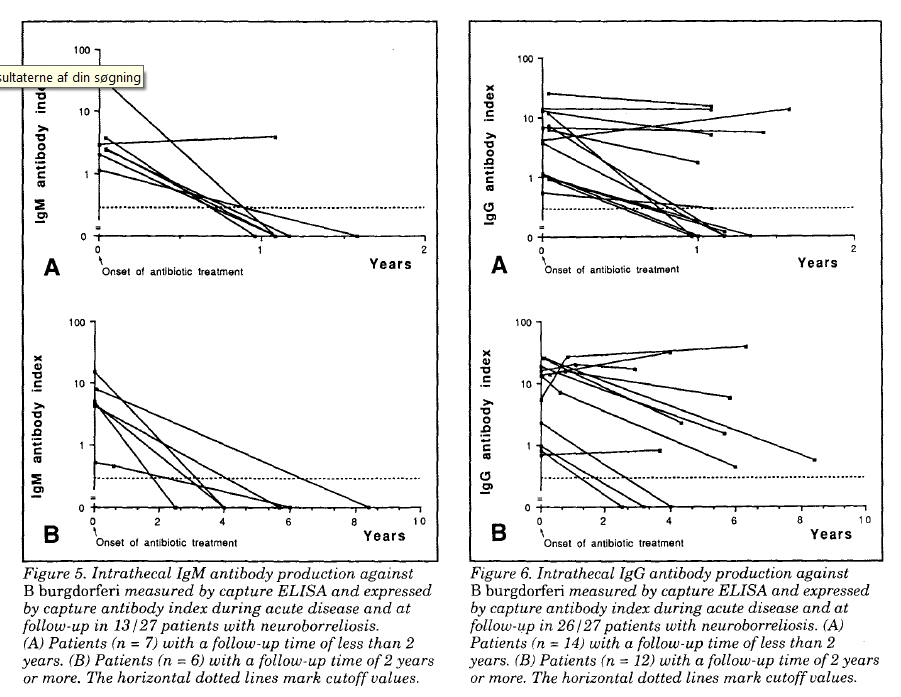
neuroborreliosis cases yearly are registred officially, of
which "only" ~ 10% (10-20 pt.) yearly (the % of possible relapses
in Denmark was deducted from Hansen and Lebech, Brain 1992; others
researchers find up to 20% relapses after recommended
treatment) may relapse / have persistent Borrelia
infection ... because of much larger number of patients in
need, these laboratories can afford to run an array
of other supplementing tests, including PCR, also for other
(tickborne) co-infections, which those patients that relapse from
Borreliosis must also be investigated thoroughly for, of course!